About Food Is Medicine @ Tufts
Food is Medicine
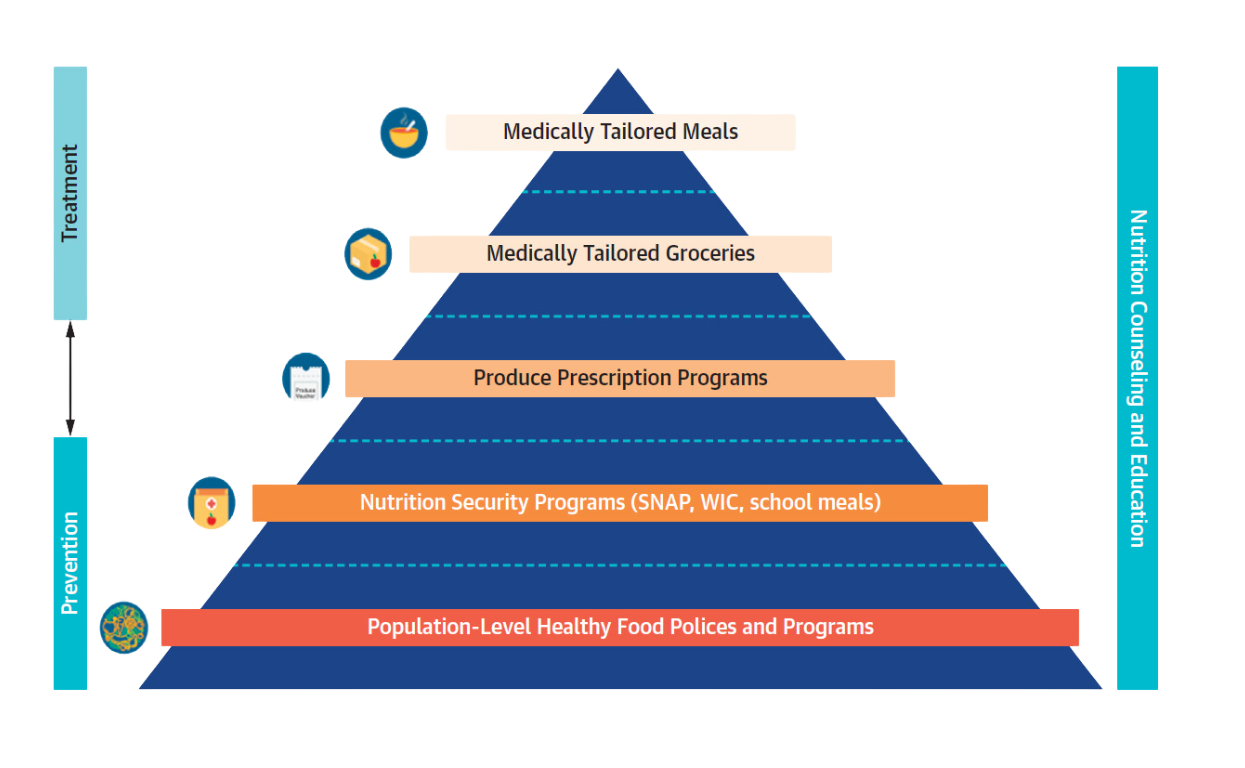
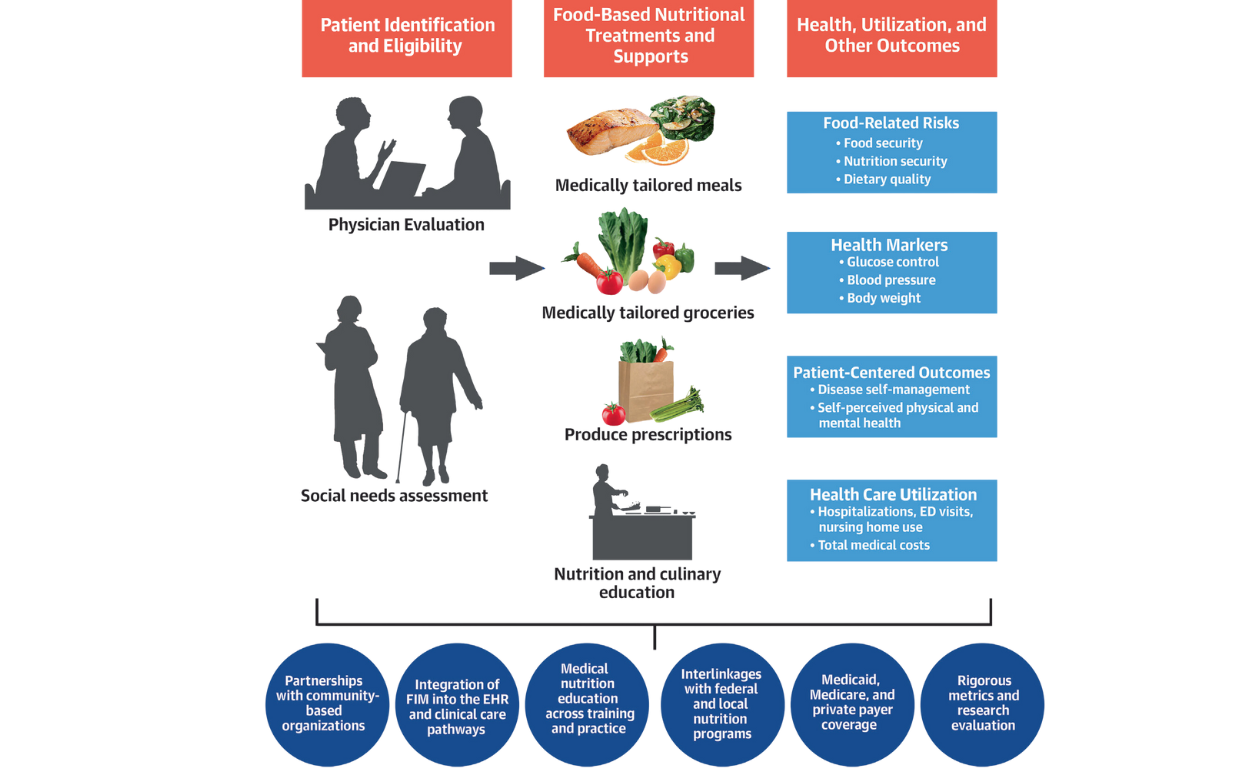
Food is Medicine (FIM) programs integrate food-based nutritional interventions into healthcare to treat or prevent disease and advance health equity. These are health sector strategies that prescribe medically tailored meals, groceries, or produce to support disease management and optimal well-being, based on the presence of a specific health condition as well as social needs. FIM programs leverage RDN expertise and offer culturally appropriate, often digital nutrition and culinary education to patients.
Mozaffarian D, et al. J Am Coll Cardiol. 2024;83(8):843–864
Supportive FIM efforts include incorporation of food and nutrition security screening and clinical care and referral pathways into the electronic health record; medical nutrition education for doctors and other providers; and policy advances to support reimbursement and scaling. FIM further leverages the major federal nutrition programs and population-level healthy food policies and programs.
FIM interventions hold great promise by emphasizing both nutrition security and health equity, while also addressing food insecurity, financial strain, and disease management.
Learn more about FIM in this fact sheet.
The Food is Medicine Institute
The Food is Medicine Institute (FIMI) is a university-wide collaborative effort based at the Friedman School of Nutrition Science and Policy, bringing together experts from across disciplines with other local and national collaborators to advance food is medicine research, training, patient care, and community and policy engagement. Tufts is the leading academic institution globally for advancing FIM, engaging in multiple large FIM interventional trials in collaboration with health care systems, extensive policy and comparative effectiveness analysis, and more. The first-of-its-kind Institute serves as a catalyst to drive change, improve health, reduce health disparities, and create a more equitable and resilient health care system that recognizes the power of nourishing food.
Vision
FIMI envisions a world where consumption of nutritious food is recognized as a fundamental component of health and health care and where all people and communities have the knowledge, resources, and support to achieve optimal health and health equity through nourishing food
NETWORKING AND COLLABORATION
FIMI will look to administer a network of collaborative efforts to implement, evaluate, and integrate food-based nutritional interventions and education to promote health, well-being, and health equity through innovative research, training, patient care, policy development, and community engagement. This collaboration will serve as a local and national catalyst to drive change, improve health, reduce health disparities, and create a more equitable and resilient healthcare system that recognizes the power of food as medicine. More information is forthcoming.
Areas of Focus
- Interventions like medically tailored meals, medically tailored groceries, and produce prescriptions, in combination with nutrition and culinary education, integration of other nutrition security programs (e.g., SNAP, WIC, school meals, meals on wheels), and consideration of cultural relevance.
- Integration of FIM into electronic health care records and care flow.
- Interdisciplinary nutrition education and training for healthcare professionals, emphasizing FIM interventions and integrating cognitive learning theory, digital education, and relevance to diverse populations.
- Development of appropriate FIM quality metrics and reimbursement pathways.
- FIM policy analysis, evidence synthesis, and advocacy.
- Community, private sector, and public health engagement around FIM programs and supportive policies and practices (e.g., education, economic mobility).
Activities
Who We Are
Learn more about the experts and researchers from the Food is Medicine Institute who are leading this work.

